This post will answer critics who say: “Borderlines are not motivated to attend therapy. Borderline patients don’t stay in treatment. At best, therapy can manage but not cure BPD.”
These statements are absolutely false. Yet these myths continue to appear online, often being communicated to people recently diagnosed. As the studies below demonstrate, most people diagnosed with BPD do want help, most will stay in good treatment, and most do recover to different degrees.
Earlier posts have elaborated my dim view of the (non) validity of the BPD diagnosis. Since it cites studies using the BPD construct, this post might be viewed as hypocritical. That may be a valid criticism! Nevertheless, these studies provide evidence that people with “borderline symptoms”, however defined, can be motivated and recover both with and without therapy
Study 1: 88 Borderline Patients Treated Twice a Week for Three Years
Highlights: Led by Josephine Giesen at Maastricht University, Dutch researchers treated 88 borderline patients for three years with twice-weekly psychotherapy. Patients were randomly assigned to either Schema-Focused Therapy or Transference-Focused Psychotherapy, which are described in detail below.
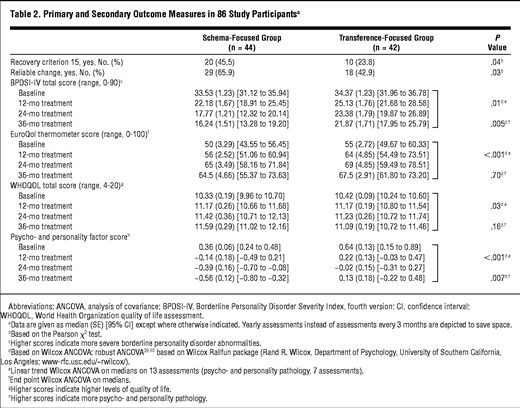
After three years, a large majority of patients showed significant improvement, with many considered fully recovered and no longer diagnosable as borderline. In the group of 45 patients undergoing Schema-Focused therapy, more than half were no longer diagnosable as borderline after three years, and many more had improved significantly.
The researchers commented, “These treatments demonstrate that patients with BPD can be motivated for and continue prolonged outpatient treatment… Three years of treatment proved to bring about a significant change in patients’ personality, shown by reductions in all BPD symptoms, increases in quality of life, and changes in associated personality features.”
Here are details from the study:
Patient Population: 88 Dutch patients diagnosed with BPD. Average age around 30 years, with most patients in their 20s or 30s. Over 90% of patients were female. The group had average educational levels for Holland; about half had attended some college or completed a degree. As for functioning before treatment, around 50% were on state disability, 20% were working, and the remainder were students or stay-at-home wives/mothers.
Trauma in Patients’ Histories: Over 85% of the patients reported childhood physical abuse. About 90% reported childhood emotional abuse or neglect. More than 60% also reported sexual abuse. Over half the patients had seriously contemplated or attempted suicide within three months before treatment. About three-quarters were taking some type of psychiatric medication.
Intervention: For a three-year period, patients attended two 50-minute sessions per week of either Schema-Focused Therapy (SFT) or Transference-Focused Psychotherapy (TFP). Treatment occurred at outpatient medical centers in four Dutch cities. The type of therapy given was randomized.
Definition of Schema-Focused Therapy: SFT is a psychodynamic treatment which assumes the existence of schemas (mental models of relationships) expressed in pervasive patterns of thinking, feeling, and behaving. The distinguished modes in BPD are detached protector, punitive parent, abandoned/abused child, and angry/impulsive child. Change is achieved through a range of behavioral, cognitive, and experiential techniques that focus on (1) the therapeutic relationship, (2) daily life outside therapy and (3) past traumatic experiences. Recovery in SFT is achieved when dysfunctional schemas no longer control the patient’s life.
Definition of Transference-Focused Therapy: TFP is a psychoanalytically-derived therapy which focuses on the transference relationship between patient and therapist. Prominent techniques are exploration, confrontation, and interpretation. Recovery in TFP is reached when good and bad representations of self and others are integrated and when fixed primitive internalized object relations are resolved.
Therapist Composition: 44 different therapists treated the 88 patients. Over 90% of the therapists had doctoral or master’s level training. All therapists had previous treatment experience with BPD patients. Therapists averaged 10 years of experience working with borderline individuals.
Outcome Measures: Patient progress was assessed every 3 months for 3 years. The primary outcome measure was the BPDSI-IV, a 70-item scale measuring the severity and frequency of borderline symptoms. Patients also completed regular quality-of-life questionnaires. These included the World Health Organization quality of life assessment, a 100-item questionnaire covering level of satisfaction with interpersonal relationships, level of independent functioning, psychological wellbeing, and physical health.
Dropout Rate: Of 45 patients treated with Schema Therapy, only 11 dropped out during the entire 3-year period. So 75% of this group persevered in intensive therapy for at least three years.
Of 43 patients treated with Transference-Focused Therapy, 18 dropped out during the 3-year period. However, the study notes that 10 of these 18 drop outs disliked the therapy method or their therapist, and 5 of 18 had issues around TFP’s method of enforcing contracts. Many of these dropouts occurred in the first few months. In my opinion, TFP is a more rigid, less effective form of treatment, and so it’s unsurprising that more patients dropped out. There’s no reason these patients couldn’t do better in another treatment.
Understanding Improvement in these BPD Patients
So how was improvement in these patients measured?
To answer this, one has to understand the measures used in the study. The primary gauge was the BPDSI-IV scale, which was filled out by patients every three months for three years. The BPDSI consists of 70 items arranged in 9 subscales. For each of the 9 DSM symptoms, 7-8 questions are asked to determine how severe and frequent the behaviors/feelings have been over the past three months, from the patient’s perspective. Each question is rated on an 11-point scale, running from 0 (never, not at all, low) to 10 (daily, very intensely, high).
For example, several questions would ask about the intensity/frequency of a patient’s feelings of emptiness (DSM BPD criteria #7), several questions would ask about the intensity/frequency of a patient’s suicidal thinking/behavior (DSM criteria #5), several questions would ask about how unstable or intense the patient feels their relationships to be (criteria #2), and so on.
The scores relating to each symptom are then averaged, producing an overall rating for that symptom. (For example, the scores for all questions about emptiness would be averaged to produce one “emptiness score”, a number between 0 and 10.) These 9 average rating for the 9 symptoms (numbers between 0 and 10) are added up to give a “BPDSI-IV” score, which represents the severity of the patient’s borderline problems over the last three months. This number will be anywhere between 0 and 90, with 0 being perfect mental health and 90 being the severest borderline disorder.
Although I dislike the BPD diagnosis, I don’t mind the method used in this study, because it involves asking the “borderline” patients how they feel. In other words, the BPDSI scale is not a judgment by clinicians, it’s a report from patients.
Improvement in BPDSI and Quality of Life Scales during the first year:
With this understanding in mind, here is how the patients did over the first year:
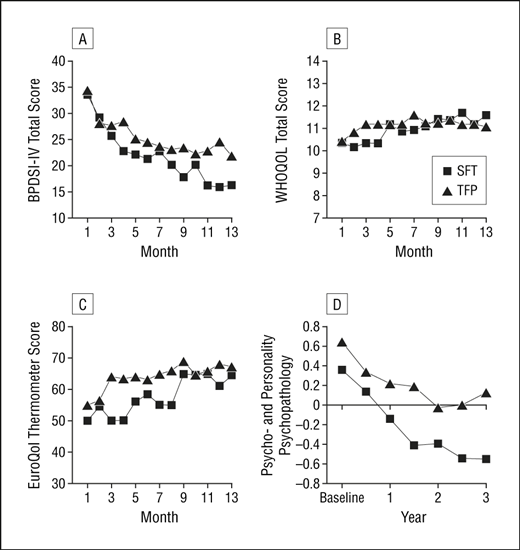
In the top left graph, we see that in the schema therapy group (line with squares), the patients started out at an average BPDSI rating of around 35 (out of 90, with 90 being the most severe, representing the worst rating for each of the 9 BPD symptoms), but this had dropped to almost 15 by the end of the first year. The patients in the transference therapy group also improved, but a little less so.
The other measures are as follows:
The bottom left Euro-QOL scale is a measure of the patient’s subjective feeling of well-being on a scale from 0 to 100, with 100 being the best. We can see that it improved significantly for both patient groups over the first year.
The top right WHO-QOL scale is another quality of life scale, and the bottom right scale is a measure of psychopathology, neither of which I researched in depth. But the trend lines in each case are positive
Outcome In Terms of Symptom Reduction
Now let’s take a look at how the patients did in terms of each of the 9 BPD symptoms. Here is the graph of the treatment groups’ averages for symptom severity over time:
The left-hand numbers on each graph represent the average BPDSI rating for the group for that symptom. For example, for item C (top right), the “Identity Disturbance” rating (DSM symptom #3) started at an average of 5 out of a worst-possible rating of 10. This rating is an average for all the patients in the group. It then drops to an average of less than 2 out of 10 after the first year, an impressive reduction.
Average group ratings over time for all 9 BPD symptoms can be seen. From the top left, the items are: Abandonment score, Unstable Relationships sore, Identity Disturbance, Impulsivity, Suicidality, Emotional Instability, Emptiness, Anger, and Paranoid/Dissociative Tendencies. All of these ratings are from the patients’ perspective. The reader can see that in every case the trend is positive (symptoms getting less intense and frequent).
Detailed Outcomes Over Three Years
Lastly, here is data showing the patients’ progress over three years:
We can see that the patients improved a lot in the first two years, and tended to maintain that improvement between years two and three. I don’t interpret this pessimistically. After a significant period of early improvement, there is often a time where a person works to become more secure in their new level of functioning and relating. This may partly account for the “leveling off” of the scores between years two and three. If the patients continued in treatment (or on their own), they could improve further.
After three years, at least half of the Schema therapy group’s patients had recovered to the point where they felt well enough to no longer be considered “borderline”, and more than two-thirds were considered highly improved. “Recovery” was defined in this study as achieving a BPDSI score of lower than 15 out of 90, and maintaining that level through the end of the study. Other patients who improved a lot (e.g. going from a BPDSI rating of 50+ down to 25 or 20) would only barely be diagnosable as borderline, even if they weren’t considered “fully recovered”.
These studies tend to be very binary (e.g. people are either “recovered” or “not recovered”, but reality is not like that). It’s important to remember that improvement is a process; it’s never all or nothing!
Jeffrey Young’s Comments
Dr. Jeffrey Young of Columbia University is the developer of Schema Therapy for BPD. He commented on this study as follows: “With Schema Therapy, patients with BPD are now breaking free from lives of chaos and misery. Not only are they learning skills to stop self-harming behaviors, as they have with Dialectical Behavior Therapy, but a high percentage of BPD patients are finally making deeper personality changes that have not been possible until now.”
For Young, this study demonstrates that therapy for BPD can lead to full recovery, and that longer-term psychodynamic therapy can be very effective. However, his comment might be a little grandiose, as people with borderline symptoms made “deeper personality changes” long before he invented Schema Therapy.
Young’s group added that this intensive schema therapy may have advantages over Dialectical Behavioral Therapy. According to Young, “DBT relieves many of the self-destructive behavioral symptoms of the disorder, but may not reduce other core symptoms, especially those related to deeper personality change.”
Interestingly, Young noted that part of schema therapy’s success may involve its emphasis on “limited reparenting”, i.e. on the creation of a loving relationship between patient and therapist. This is closely related to what I discussed in article #10, in the phase of Therapeutic Symbiosis:
More information is available at www.schematherapy.com, and I adapted the statements above from this webpage – http://www.schematherapy.com/id316.htm
My View on Schema Therapy
I am by no means an expert on Schema Therapy, and I have no affiliation with Dr. Young. My understanding is that SFT involves a mix of cognitive-behavioral and psychodynamic techniques. It focuses on building a positive therapeutic relationship, on better managing daily life, and on working through past traumatic experiences. These elements are common to most therapies.
Schema therapy also contains an object-relations (psychoanalytic) foundation, in that it conceptualizes the borderline patient as using “schemas” in their mind to represent and relate to themselves and others. Examples of these are punishing parent and angry child, uncaring parent and abandoned child, etc.
Schema therapy helps the borderline patient understand how these faulty models developed – often due to trauma and poor parenting – and to stop the replaying of negative past interactions from destroying the potential for new, better relationships in the present. In this sense, it is based on Fairbairn’s object relations model, discussed below.
As Fairbairn said, “The psychotherapist is the true successor to the exorcist. His business is not to pronounce the forgiveness of sins, but to cast out devils.” 🙂
How Individuals Get Lost in Group Studies
My biggest criticism of this type of study is that it obscures individuals’ experiences behind numbers and averages. Of course, its intent is not to provide individual detail. But,I would like to hear from individual patients what their life experience was like at the end of treatment compared to the beginning. I’m sure many would speak very positively about their progress. Since we don’t have that, I recommend the reader to case studies referenced in these posts:
https://bpdtransformation.wordpress.com/2013/12/15/what-to-do-if-you-are-diagnosed-with-bpd/
https://bpdtransformation.wordpress.com/2014/08/17/18-heroes-of-bpd-jeffrey-seinfeld/
The Mystery of Why People Are Still Pessimistic About BPD Treatment
In the bigger picture, this study’s results are obvious. Intensive help helps people, just like the sky is blue and the sun rises in the east. “Borderlines” are no exception to this. If they can access effective support – and are given a reasonable sense of hope – people diagnosed with BPD will do very well. What we need to be doing is getting more people access to effective treatment, and leaving behind the outdated myths that BPD is untreatable or incurable.
It’s amazing how such common sense escapes people who say, “borderlines don’t seek help, borderlines won’t stay in treatment, borderlines can’t be cured etc.” In my opinion, they are about as well-informed as people who think the Earth is flat.
Here is the original study of the 88 Dutch patients: http://archpsyc.jamanetwork.com/article.aspx?articleid=209673
Other Studies on Psychotherapy’s Effectiveness for BPD
This study is one of many investigating psychotherapy’s effect on BPD. Below are additional examples, one from a hospital outpatient program, one from DBT, and one comparing different psychotherapies:
Treatment of Borderline Personality Disorder with Psychoanalytically-Oriented Partial Hospitalization, An 18 Month Follow-up: http://psychiatryonline.org/doi/abs/10.1176/appi.ajp.158.1.36
Dialectical Behavior Therapy for Patients with Borderline Personality Disorder and Drug Dependence: http://www.ncbi.nlm.nih.gov/pubmed/10598211
Evaluating Three Treatments for BPD: A Multi-wave Study: http://www.borderlinedisorders.com/images/AJPRCT.pdf
All of these studies show positive results. Again, this is not rocket science – good treatment helps people diagnosed with BPD!
What If Borderlines Don’t Get Good Therapy?
But what is people diagnosed with BPD don’t get good long-term psychotherapy? Do they inevitably do badly?
No.
Several studies address this question, including the one summarized below:
http://www.borderlinedisorders.com/images/AJPRCT.pdf
Here are the highlights of this study:
Study 2: 290 Borderline Patients In Massachusetts
Patient Population: 290 patients diagnosed with BPD, assessed at McLean Hospital in Massachusetts. They were first treated as inpatients during brief hospital stays.
Method of Study: This was a longitudinal-observational study. The patients were interviewed every two years for at least 10 consecutive years, starting in the early 1990s. During interviews, their level of functioning in work/school, satisfaction with interpersonal relationships, and degree and frequency of borderline symptoms were measured. After 10 years, 90% of the original cohort of 290 patients were still participating.
Therefore, this study followed the “natural course” of BPD. This medical-model idea is misleading (the notion that BPD has a “natural course”), but I won’t go into that now. Suffice it to say that the researchers in this study did not “treat” the patients – they just followed them after hospitalization and went to great lengths to see how they were doing every two years.
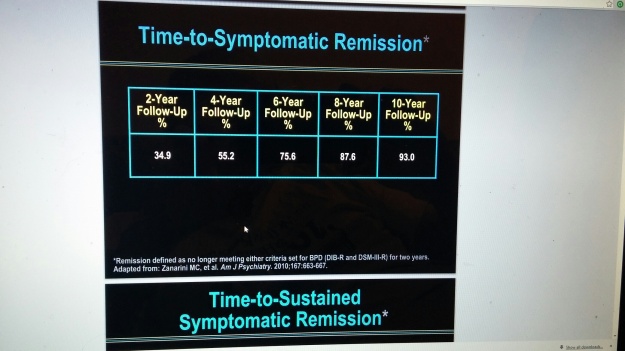
High Remission of Symptoms: After 10 years, 93% of the formerly borderline patients had experienced at least two consecutive years during which they no longer qualified for the BPD diagnosis, according to DSM criteria:
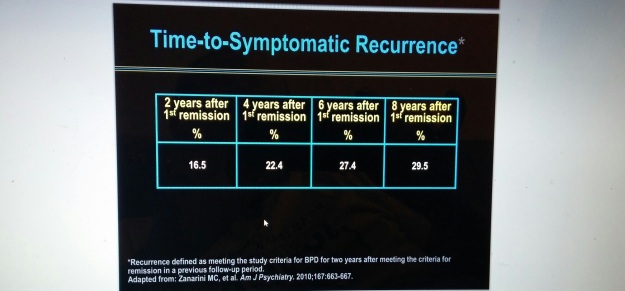
Low Recurrence of Symptoms: After 10 years, among the 93% of patients who achieved symptomatic remission, only 29% became “borderline” again. In other words, once they improved to the point of no longer being diagnosable as borderline, a large majority did not get worse and become “borderline” again:
Good Social and Work Functioning: After 10 years, 78% of patients had achieved good psychosocial functioning – defined as good performance in a job for at least two years, along with at least one emotionally sustaining relationship with a partner or friend: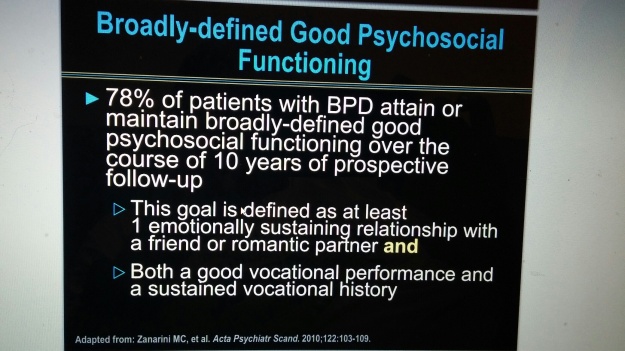
To me this last slide is questionable, as it’s not clear how “good work performance” was defined (and a certain period of work is not a prerequisite for “recovery”, anyway). Nevertheless, this study shows how, in a group of previously hospitalized borderlines, most people improve to the point where they are able to function in a job and have an intimate relationship. Again, the study authors provided these patients with no treatment beyond brief hospitalization, although many probably sought help on their own.
Other Longitudinal Studies of Borderlines Are Also Positive
There are many other ways to critique this study; for example, one could say it only applies to “borderlines” in the northeastern United States who went through McLean hospital. However, other studies following borderline patients for decades reach similar conclusions.
These include Thomas McGlashan’s Chestnut Lodge study (Maryland, USA), Michael Stone’s “Fate of Borderline Patients” study (New York, USA), and Joel Paris’ longitudinal study of borderlines (Montreal, Canada). All of these studies concluded that a large majority of borderline patients improved significantly, and many recovered in the long term. Collectively these studies included over a thousand patients. These studies can be found by searching online, as well as through the books by McGlashan, Stone, and Paris on Amazon.
The Limitations of Naturalistic Studies Based on Diagnosis
The anti-psychiatry side of me says that these longitudinal studies reveal what a meaningless and unreliable diagnosis BPD is. It doesn’t make sense that some percentage of people are initially borderline, then at varying points in time they are suddenly no longer borderline, then a few of them are borderline again, and so on.
Maybe BPD was never a valid illness to begin with. But such common sense seems to escape Harvard-educated researchers like Zanarini 🙂 Then again, to admit that what they’re studying is an unscientific fabrication wouldn’t be great for their careers, nor for receiving funding from the National Institute of Mental Health.
Although these studies have flaws, I hope readers will see that people diagnosed with BPD do seek help, and that they can recover to be emotionally well and free of “borderline” symptoms. These are not just opinions. They’re facts.
On The Nature of Quasi-Experiments
Lastly, it is important to understand that these studies – like most in psychology – are quasi-experimental. This means they are not perfectly controlled experiments, because when studying human beings many factors simply cannot be controlled. One can never study a person as reliably as one studies solar radiation or the molecular structure of uranium.
No one quasi-study can “prove” a point definitively. Nevertheless, quasi-experimental studies can estimate the effect of a variable(s) on a group of people under certain conditions. And a pattern of quasi-studies with similar results can show that something real is happening
These studies should also not be interpreted as applying to any particular person. Rather, they are averages of many different people’s outcomes, and only have meaning on a group level.
Wow, I am exhausted thinking about all this data. Time to get a beer!
——————————–
I welcome any correspondance at bpdtransformation@gmail.com
If you are struggling with BPD yourself or are trying to help a borderline individual, I would be happy to listen to your story and provide feedback if possible. Feel free to provide constructive criticism of this site also.
This article is the opinion of a non-professional layperson, and should not be taken as medical advice or as the view of a therapist who is professionally qualified to treat Borderline Personality Disorder or any other mental health condition. Readers should consult with a qualified mental health professional before undertaking any treatment.
– Edward Dantes


Reblogged this on Awesome Elo and commented:
This is some really great information and I can personally attest to some of this information
LikeLike
Thank you and glad you can attest to getting better too!
LikeLike
I second Elo and I can attest to healing taking place and recovery happening from doing deep emotive based healing and growth work with a facilitator. I worked within this particular paradigm: http://brightage.org/
I just wish you had some actual recommended facilitators in my area I could consider to see – as I’m ready to take my emotional growth and healing to the next level!
LikeLike
Thanks Ian. I looked at that website. It looks a lot more positive than the DSM/psychiatry’s approach 🙂 Although I’m not sure how hard it is to be more positive than them! 🙂
Yes there is still a lack of resources like the therapy discussed in this article. But at least it is encouraging that “doing well”, variously defined, is possible when doing with BPD symptoms. I also don’t think one has to have a certain type of therapy to get better. A lot of the problem for people is that there’s so much unwarranted pessimism out there about “borderlines” and other mental “illnesses”. These negative beliefs are like demons that need to be exorcised.
LikeLike
OH – and LOVE the new backdrop on your website!
LikeLike
Thanks several people told me the last one was horrible 🙂 (the diagonal colorful stripes)
I love astronomy so you are viewing a bunch of galaxies there…
LikeLike
This is excellent. The more I learn about “personality disorders”, the more I question the whole concept. Diagnoses appear and disappear from the DSM, patients are labeled with multiple contradictory disorders at the same time, checklists allow a single label to be applied to people with no symptoms in common, and some diagnoses are apparently linked to infantile brain damage while others are not…. And supposedly incurable disorders turn out to be curable after all, while patients are not informed of this.
What really sickens me is that patients who have sought treatment in desperation are labeled as not wanting to change because some of the treatment approaches are flawed. It’s like the diet industry blaming overweight clients as uncooperative because the diets don’t work.
LikeLike
Thanks I always appreciate your comments. Diets is something I’ve read about and been interested in. Obviously, humans are not adapted (yet) evolutionarily to deal with the sedentary lifestyles and high-glucose/carbohydrate diets that we have today. Rather, as hunter gatherer-cavemen tens of thousands of years ago, our priority was to eat as much as possible in case we had to wait a long time for our next meal. It’s difficult to shift from that orientation within a few millenia or centuries, biologically-evolutionarily speaking. Although I think individual people can do it.
I remember reading an article saying that Weightwatchers is the only program that’s been proven to help people lose weight and keep it off. I’m not sure whether that’s true or not, but it was encouraging that at least there’s something.
And yes I agree with you that it’s ridiculous how people are negatively labeled and judged as being unwilling to change. Of course they want to change, they may just not know how! Treatment professionals should have the humility to admit it if their approaches aren’t working well. And to give them credit some of them do this, but not enough yet.
A good metaphor for the current diagnostic system might be the way in which Newtonian physics totally failed to describe space and time accurately, and a new science (relativity, Einstein) was needed to provide understanding. We need something like that for emotional distress. Right now hopefully more and more people can come to realize that the current system of diagnosing/treating mental “illnesses” is fatally flawed. If enough people understand that, it will doom the current system of psychiatry and cause its collapse.
LikeLiked by 1 person
I have finally had time to read, once again with interest. Im trying to get daughter K to speak ..see someone. The graphs kind of lost me, but once more very informative Edward.
LikeLike
Ok good. How are things going with K now?
LikeLiked by 1 person
She’s a bit hazy from the seizures, her memory still not good, feeling odd, but I think she hasn’t relaxed since coming out on Friday. I have managed to get in contact with a psychoanalyst, she said she would be phoning K today to have a chat. She sees BP’s, practices DBT, does hypnotherapy. She doesn’t practice Schematic though. On email she sounded quite nice and caring, saying she follows up her patients with two ph calls a week to check in on them. This is more support than the clinic provided. I hope she can see someone..to talk things out…not hanks for asking Edward.
LikeLike
Man, really good stuff. I’ve been blogging about my experienced with BPD over the years and even wrote a book on it, definitely wish there were more people like you showing that BPD is much more complex than just ‘BPD’. I mean it’s like 50 issues under one umbrella in a sense lol. Anyways, keep up the good work and glad to see some science backing up everything I’ve been explaining for years.
LikeLike
I second that Rick! Edward’s blog is definitely one I can relate with and can attest myself that true healing and recovery is possible through psycho-emotional growth work.
LikeLike
Right, and the “umbrella” (BPD) is really a carefully crafted illusion. Thank you for your comment Rick and I’m glad to see there is someone else that thinks similarly. I will check out more of your writing and book.
LikeLike
Yup – once one deals with the root emotive congestion then the label is moot. BPD is only to group symptoms and patterns and once the root repressed emotion is felt through then a person changes from the inside out and no longer has to have those symptoms to compensate or defend oneself with.
LikeLike
My point tries to go even deeper than that. Even before one deals with the “root emotive congestion”, the label BPD is moot, non-existent and invalid. In other words, BPD is an illusory grouping of symptoms. There is no proof that “BPD” describes a pattern of symptoms that reliably occurs together from person to person (i.e. more frequently than might be expected if only chance/coincidence were involved). If a description like this is not “reliable”, then it cannot be valid. Many people just accept BPD without ever questioning whether it (the diagnosis, not the symptoms) really exists.
But yes I definitely agree with your point that when troublesome emotions are worked out, that is always a good thing and that promotes growth because one is no longer having to devote energy to defense.
LikeLike
WOW – I guess I didn’t get that completely. Agreed!
LikeLike
Hi Edward,
I want to thank you for this site. It makes a big difference in all blogs and articles about BPD because of your attitude and positive approach I totaly agree with.
I was raised by parents who both suffer from abusive childhood experience and never were treated, I developed symptoms of BPD and was diagnosed 11 years ago. What I see is not BPD, I simply see only survival system that is more detrimental than helpful in the long run.
What really helped me were spiritual community (especially empathy and compassion) and therapy like One Brain (for those who are interested http://kinesiologie.homestead.com/englishsumm.html, http://www.3in1concepts.us/creators.php) and Somatic Experience (creator Peter Levine). Both therapy approaches address and heal childhood trauma! Both are holistic so they work with body-mind-soul. I don’t run a blog and because I haven’t found till now anyone with BPD being treated with this kind of therapy I thought I mention it here 🙂
(sorry for any grammar mistakes, I’m not English native speaker :))
LikeLike
Hi Judith, thank you for your comment. I know Peter Levine and his book Waking the Tiger. There’s a good approach called Bioenergetics by Alexander Lowen, and it’s predecessor Character Analysis by Wilhelm Reich. These are both focused on how trauma gets stored in the body in chronic muscular tensions and they are truly mind body approaches I’d say.
I agree with you that what is called bpd is a survival system that is the best a person can do at the time to cope with a difficult situation. As you know I don’t find it valid or useful to speak of “it” (the bpd diagnosis) as a valid entity that actually exists, because really only symptoms of various kinds exist, not some disorder based on an artificial grouping of symptoms. If you like the idea of the survival system, also check out Donald Kalsched and his beautiful book the Inner World of Trauma. He specifically calls Bpd a survival or self-preservation system.
What is your first language?
LikeLike
Thank you Edward for the recommended readings 🙂
I remember, probably you, describing how important is for those with BPD to find hope and validation. I can attest to that and I would just add to that possibilities/options. I believe in power of feelings and in rewriting your trauma story on a cellular level which Somatic experience therapy enables and thus helps in faster recovery. Pesso-Boyden group therapy was also recommended by my therapist as a therapy that helps specifically replenish those needs that never have been met in childhood (trust, empathy, validation, safety,…).
My first language is Czech 🙂
LikeLike
Ok cool. I once lived in Warsaw Poland and I visited Czech Rep briefly. Thanks again for your thoughts on all this
LikeLike
Reblogged this on schizoaffectiveandocd.
LikeLike
Reblogged this on Lucky Otters Haven and commented:
BPDTransformation used to be one of my frequent commenters but has not posted anything in his blog in over a year, or made any more comments. Edward (his real name) wrote fascinating, intelligent, and extremely well researched articles about BPD, which he was diagnosed with. At some point he came to believe BPD was a bogus diagnosis, a catchall for an array of symptoms that weren’t easily classified or understood. (Some people believe BPD and C-PTSD are the same disorder, which does make sense).
Edward, who became BPD-free, writes here about how motivated many borderlines are to recover, and how effective psychotherapy can be in healing this disorder. This flies in the face of the common belief that because it’s a Cluster B personality disorder, that BPD is just something you have to resign to yourself to having forever.
The article, like most of Edward’s articles, is a bit on the scholarly side, but is still a very good read.
LikeLike
Pingback: Proof that borderlines are motivated for psychotherapy and can fully recover (reblog: BPDTransformation) – Down the Rabbit Hole